High Complexity Units
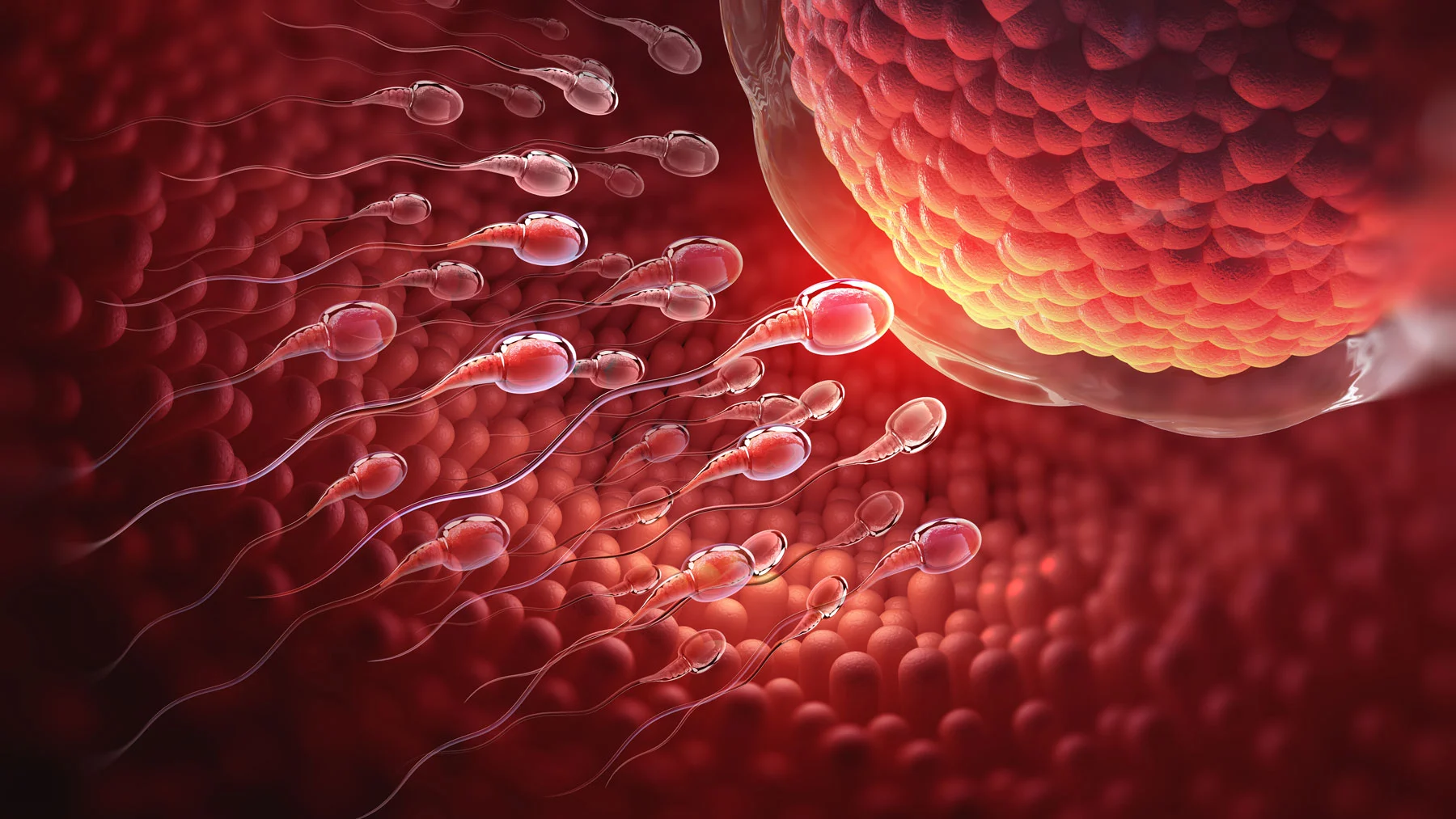
Male fertility
Ginefiv’s Male Fertility Unit is a high complexity unit that enables us to offer specialised and personalised care to males with issues that are directly or indirectly related to infertility.
This unit provides an assessment of the different problems (erectile dysfunction, varicocele, hypergonadism, azoospermia, prostatitis, etc.) using a multi-disciplinary focus which allows us to better address the disease and therefore achieve better results in assisted reproduction techniques.
To do this, our male fertility high complexity unit works in coordination with the following units:
- Andrology
- Urology
- Advanced genetics
This is the only way that we can offer our patients the best solutions to their infertility,
with the highest guarantees of success.
It is essential to use the most advanced diagnosis techniques and therapies so we can ensure the highest probability that a male can have children with their own genes, avoiding the use of donor semen, barring highly exceptional cases
How can we help you?

1. Obtaining testicular spermatozoa: When carrying out assisted reproduction, one of the more complex situations wemight find in the treatment of infertility caused by severe male factor is the absenceof spermatozoa or a low sperm count in the ejaculate.
In cases like these, we have to consider seeking out the spermatozoa where they are produced, i.e. in the testicles, using procedures with maximum guarantees of effectiveness and safety.
To do this, we have various spermatozoa collection techniques which we can select depending on the specific case.
- TESE: a biopsy during which we obtain testicular tissue.
- TESA: a puncture process with a fine needle that is used to collect testicular spermatozoa.
- MicroTESE: on occasion, azoospermia occurs due to intratesticular failure to produce spermatozoa (secretor azoospermia). In these cases, a considerable percentage of patients have small zones in the testicles which do in fact produce spermatozoa. To locate these zones more easily and to be able to gather the male gametes, we use microsurgery with image magnification, allowing us to locate the tubules in which there is a high probability of sperm production.
2. Selecting testicular spermatozoa: Having obtained the sample, we ensure that the laboratory processes for spermatozoa selection are the most suited to each case. From the application of sorting techniques (Fertile chip, MACS, etc.) to the time-consuming systematic search for spermatozoa in the testicular parenchyma.
3. Genetic testing: Genetic testing of males is performed to help with the offering of the most suitable prognostics and to reduce risks for the future newborn.