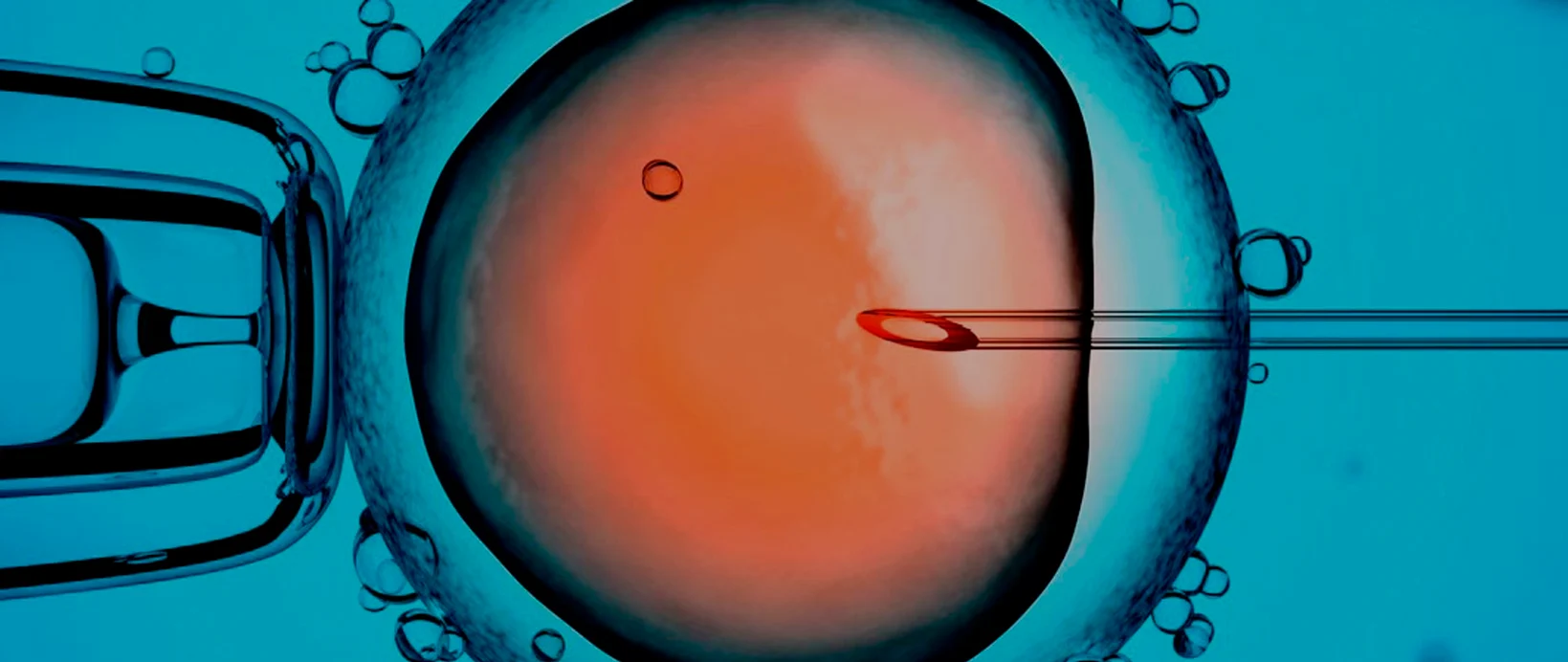
Assisted reproduction
Mini IVF or mild IVF
Mini IVF, also known as soft or mild IVF, is a variation of conventional in vitro fertilisation but it is unique in that it involves the use of a more gentle ovarian stimulation protocol. This requires administering the patient a minimal amount of hormonal medication to stimulate the ovaries. The rest of the steps in this technique are identical to conventional IVF.
Mini or mild IVF is an assisted reproduction technique that is especially suited to patients who have a good prognosis and would prefer not to undergo an intense stimulation. It is also increasingly used by patients who have a poor response, i.e. patients for who increasing the dose of their medication during conventional stimulation does not lead to an improved response but for whom a milder dose can achieve an equally good or better response.

The differences between Mini IVF and conventional IVF:
What are the advantages of Mini IVF?
It is more comfortable:
The main advantage offered by this procedure is the lower doses of gonadotropins and therefore increased comfort.
Hormonal medication is administered orally or via injections and seeing as a smaller amount is required, mini IVF is more comfortable for the patient and drastically reduces the stress caused by the treatment.
It avoids the need to freeze embryos:
Decreasing the medication dose and performing a mild ovarian stimulation produces a lower number of eggs. The objective of Mini IVF is, specifically, to obtain between 2 and 8 eggs instead of between 8 and 15 like in conventional IVF. This is because we turn to Mini IVF in cases in which the patient has a higher chance of pregnancy.
The result is embryos that are fewer in number but have a higher possibility of success and it is therefore normal for all them to be transferred to the patient’s uterus, with none of them needing to be frozen.
In general, patients who undergo a conventional IVF cycle usually have surplusembryos which aren’t transferred to the woman’s uterus and which arecryopreserved for possible use at a later date. In cases in which the first embryotransfer does not lead to pregnancy, the cryopreserved embryos allow us to performanother transfer, thereby increasing the chances of pregnancy from the treatment.When we determine that the patient is suitable to receive Mini IVF instead ofconventional IVF, it is generally in cases where their chance of pregnancy is greater.
It costs less:
In mild IVF, the overall cost of the hormonal medication is cheaper than in conventional IVF. Hormonal medication, which is usually one of the most expensive aspects of the treatment, is considerably reduced given that the patient’s ovaries are stimulated using a minimal amount.
In turn, the lab costs are also notably lower as we work with fewer gametes. Additionally, we eliminate the cost of freezing the embryos seeing as it is fairly unlikely that there will be any viable embryos which are not transferred to the woman’s uterus and which therefore need to be cryopreserved.
What are the disadvantages of Mini IVF?
It is only suitable for certain cases:
Mild IVF is not suitable for all patients, it can only be recommended to those whohave a very good prognosis.
There is less probability of success in absolute terms:
Although the gestation rates of Mini IVF are comparable to conventional IVF, this is due to the fact that Mini IVF is only carried out with patients with a good prognosis. We cannot say the same thing when talking in absolute terms because:
Fewer eggs are obtained:
As mentioned above, the objective of IVF is to obtain between 2 and 8 eggs, meaning that the chances of getting a healthy embryo with a good fertilisation capacity are less than when we gather between 8 and 15 eggs.
No cryopreserved embryos:
The pregnancy rates of conventional IVF are not based only on the transfer of freshembryos. Normally, patients who undergo a cycle of conventional IVF usually havesurplus embryos which are not transferred to the woman’s uterus and which arecryopreserved for possible use at a later date. In cases in which the first embryotransfer does not lead to pregnancy, the frozen embryos allow us to perform a newtransfer, thus increasing the chances that the treatment will result in pregnancy.In other words, in conventional IVF treatment the chances of pregnancy also apply tocryopreserved embryos, whilst this is not possible in Mini IVF as there are no frozenembryos.
When should the Mini IVF technique be used?
Mini IVF is especially suited to patients who fulfil any of the following requirements:
- Women aged under 35 who have a good ovarian reserve and a good prognosis.
- Women who have previously undergone IVF or artificial insemination cycles in which the ovarian response was excessive.
- Patients with a risk of ovarian hyperstimulation